In our daily practice, some diseases become so commonplace they can almost feel routine. We see them so often that we might process them quickly, without truly pausing to ask ourselves: “Do I really understand this condition from its roots?” One of the most significant of these diseases is Periodontitis.
This isn’t merely “just a simple gum inflammation.” Periodontitis is, in fact, one of the most widespread diseases globally and remains the primary cause of tooth loss in adults. The real problem is that many patients—and even some practitioners—don’t give it the attention it deserves until the situation escalates, teeth start becoming mobile, and the patient urgently comes in saying, “Doctor, please help me!”
In this article, we’re going back to basics. We’ll meticulously break down Periodontitis piece by piece, discussing its various types, stages, and precisely how to diagnose it accurately in your clinic. A deep, thorough understanding of this disease is exactly what will empower you to deliver a successful treatment plan to your patients, helping them preserve their teeth for the longest possible duration.
1. What Exactly is Periodontitis? (The Definition)
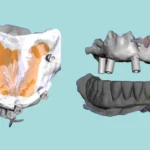
To put it very simply, this disease is a silent thief that systematically destroys the tissues holding the tooth securely in its place. These crucial tissues, collectively known as the Periodontium, are composed of four fundamental components:
-
The Gingiva (gums).
-
The Alveolar Bone, which is the bone where the tooth is actually embedded.
-
The Periodontal Ligament (PDL), connecting the tooth root to the bone.
-
The Cementum, covering the root surface.
This disease typically starts as a simple Gingivitis, which essentially means just bleeding and redness of the gums without any destruction to the underlying bone or ligaments. If this condition is left untreated and hygiene is neglected, the inflammation deepens and begins to “erode” the bone and ligaments beneath the gum line. This is the critical point where it transitions from Gingivitis to full-blown Periodontitis.
The definitive dividing line between the two is the occurrence of Clinical Attachment Loss (CAL). As long as there’s no attachment loss, the condition remains gingivitis. The moment attachment loss occurs, we have officially entered the realm of Periodontitis.
The Suspects in This Case
So, who’s responsible for this destructive process? There are three primary culprits:
-
Bacteria: The first and main suspect involves specific types of bacteria residing within dental plaque and calculus.
-
The Body’s Immune Response: The patient’s immune system’s reaction to these bacteria is what actually drives the destruction. Essentially, while the body attempts to fight off the bacteria, it inadvertently damages its own tissues along the way.
-
Risk Factors: These are the elements that exacerbate the situation, causing the disease to progress more rapidly. Examples include Smoking, Uncontrolled Diabetes, Genetic Factors, and elevated Stress levels.
2. The New Classification: Not All Periodontitis is Created Equal
To treat effectively, we must first diagnose correctly. The new global classification for periodontal diseases, established in 2017, divides the disease in a very practical manner that significantly aids us in formulating precise treatment plans (1). Let’s focus on the three most important types you’ll encounter in your practice:
2.1. Periodontitis
In the updated classification, the concepts of “Chronic” and “Aggressive” types have been abolished, merged under the single umbrella term “Periodontitis.” We then further characterize it using two key descriptors: its Stage and its Grade.
-
Staging: This describes the current severity of the destruction that has occurred. It’s divided into four stages, ranging from Stage I (mild) to Stage IV (very severe). We primarily determine this by measuring Clinical Attachment Loss (CAL) and other contributing factors.
-
Grading: This describes the predicted future rate of disease progression. It’s categorized into three grades: Grade A (slow progression), Grade B (moderate progression), and Grade C (rapid progression). This is determined based on risk factors such as smoking and diabetes.
2.2. Necrotizing Periodontitis
This is a particularly aggressive and visually alarming type. It’s characterized by tissue necrosis in both the gingiva and the bone. You’ll observe a “punched-out” appearance of the gums, intensely painful ulcers, and a distinctly foul oral odor. This condition most frequently affects individuals with significantly compromised immune systems, such as patients with AIDS or those suffering from severe malnutrition.
2.3. Periodontitis as a Manifestation of Systemic Diseases
Occasionally, Periodontitis can serve as a crucial indicator of another underlying systemic condition. This might include certain rare genetic disorders or blood diseases. Therefore, it’s absolutely vital to take a thorough medical history from every patient.
3. The Language of Perio: Essential Terminology to Master
To truly speak the language of periodontology, you must be intimately familiar with these terms:
-
Periodontal Pockets: These are the spaces that form between the tooth and the gum. We measure their depth using a periodontal probe. They can be either suprabony pockets (above the bone) or infrabony pockets (extending into the bone).
-
Clinical Attachment Loss (CAL): This is the definitive measure of destruction. It’s measured from the Cemento-Enamel Junction (CEJ) down to the base of the pocket. CAL, not just pocket depth, is what tells you precisely how much of the tooth root has become exposed beneath the gum line.
-
Morphology of Bone Loss: Radiographically, bone loss typically manifests in one of two forms. It can be Horizontal Bone Loss, meaning the bone is resorbed relatively uniformly. Alternatively, it can be Vertical Bone Loss, where bone is lost in an angular pattern adjacent to a specific tooth, leading to the formation of infrabony pockets.
-
Furcation Involvement: In molars, as the disease progresses, the bone between the roots can be resorbed. We classify this from Class I (incipient involvement) to Class III (complete through-and-through involvement of the furcation).
4. Accurate Diagnosis: Piecing Together the Puzzle (The Diagnostic Process)
A precise diagnosis is the absolute foundation upon which all treatment is built. You must gather all available information to visualize the complete picture.
What Your Patient Will Tell You (Symptoms)
-
“Doctor, my gums bleed when I brush.” Bleeding on Probing (BOP) is an initial warning sign.
-
“My gums are red and swollen.” This indicates Red and Swollen Gums.
-
“I have really bad breath that just won’t go away.” This points to Halitosis.
-
“I feel like my teeth are moving.” This suggests Tooth Mobility.
What You Will Observe (Clinical Signs)
-
Examination with a Periodontal Probe: This is your most vital tool. You’ll measure six points around each tooth to determine Probing Depth, CAL, and the presence of BOP.
-
Assessment of Tooth Mobility.
-
Evaluation of Furcation involvement in molars.
-
Assessment of Plaque and Calculus accumulation.
What Radiographs Reveal (Radiographic Findings)
Radiographs not only confirm your diagnosis but also reveal what’s hidden from direct view. You’ll identify Alveolar bone loss and determine its type (horizontal or vertical). You’ll also observe any Widening of the PDL space and can accurately assess the extent of Furcation involvement.
Conclusion: Why Accurate Diagnosis is Everything
Because without a precise diagnosis, your treatment will inevitably be haphazard. When you clearly understand the type, stage, and grade of Periodontitis, you can:
-
Formulate an Appropriate Treatment Plan: Does this case merely require Scaling and Root Planing, or are antibiotics needed, or perhaps even surgical intervention?
-
Set Realistic Patient Expectations: You’ll be able to clearly explain the exact condition of their teeth and the anticipated outcome.
-
Ensure Long-Term Treatment Success: A correct diagnosis is the crucial first step to halt the disease’s progression effectively.
Periodontitis is a serious, often silent disease. Your role as a dentist isn’t just to treat it when it reaches an advanced stage. Your more vital role is to detect it early, diagnose it correctly, and save your patient’s teeth before it’s too late.