“Doctor, I brush my teeth every single day, but I still get calculus!” How many times do we hear that exact phrase in the clinic daily? Countless patients tend to view dental calculus as simply “yellowing” or just an “unpleasant appearance,” completely unaware that it can truly be the precursor to a serious catastrophe that might lead to losing their teeth.
Our role as dentists isn’t solely to remove this calculus. Our more crucial role is to help our patients fully understand what dental calculus actually is, how it forms, and what its genuine, damaging effects are. When a patient truly grasps the severity of the problem, their commitment to oral hygiene and regular dental visits dramatically increases.
In this article, we’re going to meticulously break down the entire story of “dental calculus” from A to Z. We’ll delve into its definition, trace its step-by-step formation, explore its various types, detail its components, and most importantly, uncover the significant harms it can inflict.
What Exactly is Dental Calculus?
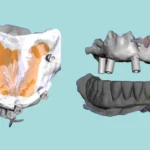
In the simplest terms, dental calculus refers to calcified deposits (or deposits well on their way to becoming calcified) that develop on tooth surfaces and any other hard structures within the oral cavity. This includes fixed and removable prostheses, and even orthodontic appliances.
Imagine that soft, sticky plaque layer as a sort of “powdered cement.” If you leave it untouched without removing it with water (meaning, without brushing and flossing), your saliva will act like water on it, transforming it into a hard, stone-like mass of “cement.” That hardened mass is dental calculus.
The Step-by-Step Journey of Calculus Formation
Calculus doesn’t just appear overnight; it’s a gradual process that unfolds over several stages:
The Beginning: The Plaque Biofilm
Everything kicks off with that sticky plaque layer, which starts forming on teeth mere minutes after brushing. This layer is essentially a highly organized colony of bacteria living within a matrix of proteins and sugars.
If this layer isn’t consistently removed through regular brushing and flossing, the bacteria within it begin to die and decompose. This decaying material then acts as a “seed” or “nucleus” for the subsequent process of mineralization.
Mineral Precipitation: The Mineral Rain of Calcium and Phosphate
Our saliva is abundantly rich in calcium and phosphate ions. When these ions encounter this “dead” plaque layer, they start to precipitate within it and bind to it.
This precipitation also receives contributions from a fluid known as Gingival Crevicular Fluid (GCF), a fluid that originates from the gums and is also mineral-rich.
The Role of Bacterial Enzymes: The Tiny Traitors
And it’s not just that! The living bacteria within the plaque actively contribute to this calcification process. They secrete enzymes such as phosphatases and proteases.
These enzymes work by breaking down the body’s natural “calcification guardians” present in saliva, like statherin and proline-rich proteins. The natural function of these guardians is to prevent indiscriminate calcification throughout the mouth. When these guardians are compromised, the path for mineral deposition becomes wide open.
The End Result: Mineral Crystal Formation
All the preceding processes ultimately lead to the formation of insoluble mineral crystals. These crystals initially begin to form within the intercellular matrix between bacterial cells, then on the bacterial surfaces themselves, and finally, inside the bacteria. This continuous process culminates in the creation of a solid, calcified mass that closely resembles bone (1).
An Important Note: The surface of dental calculus is always covered by a layer of active, uncalcified plaque biofilm. This means calculus isn’t just a dormant “stone”; it’s a “five-star hotel” for bacteria, providing a rough surface where they can thrive, multiply, and incessantly release their toxins that devastate gum tissue.
Types of Dental Calculus
Calculus isn’t a single entity. We primarily categorize it into two main types based on its location relative to the gum line, and each type possesses distinct characteristics:
Supragingival Calculus
-
Location: Found above the gingival margin. This is the type both you and your patient can easily spot.
-
Color: Typically yellowish-white, though it can darken over time due to pigments from food, beverages, and tobacco use.
-
Consistency: Tends to be less hard and somewhat brittle, making it generally easier to remove.
-
Source: Primarily nourished by minerals found in saliva.
-
Preferred Locations: It particularly loves forming near the openings of major salivary glands. This is why we consistently find it in abundance on:
-
The buccal surfaces of maxillary molars (adjacent to the opening of the parotid gland).
-
The lingual surfaces of mandibular anterior teeth (near the openings of the submandibular and sublingual glands).
-
Subgingival Calculus
-
Location: Resides below the gingival margin, deep inside the periodontal pocket. This is truly the “hidden enemy” that we can only detect with our specialized instruments.
-
Color: Significantly darker, often dark brown, black, or even greenish. This darker hue comes from blood products that seep from inflamed gingival tissues.
-
Consistency: It’s much harder and denser, adhering very strongly to the root surface, which makes it considerably more challenging to remove.
-
Source: Primarily nourished by minerals found in the Gingival Crevicular Fluid (GCF).
-
Preferred Locations: While it can form on any subgingival surface, it particularly favors interproximal surfaces due to the difficulty of cleaning these areas effectively.
Composition of Dental Calculus
What exactly is calculus made of internally? It’s a complex blend of both inorganic and organic materials:
-
Approximately 70-80% Inorganic Components:
-
Hydroxyapatite (the most common form).
-
Magnesium whitlockite.
-
Octacalcium phosphate.
-
Brushite (more frequently found in newly formed calculus).
-
-
Approximately 20-30% Organic Components:
-
Remnants of living and dead bacteria.
-
Desquamated epithelial cells.
-
Leukocytes (white blood cells).
-
An organic matrix composed of proteins, lipids, and carbohydrates derived from saliva and bacteria.
-
What Factors Increase Calculus Formation?
Not everyone forms calculus at the same rate. Several factors play a role in its acceleration:
-
Saliva Characteristics: Individuals with more viscous or scanty saliva, or saliva that’s particularly rich in calcium and phosphate, tend to form calculus more rapidly.
-
Dietary Habits: A diet high in soft foods and sugars promotes greater plaque accumulation, thereby increasing the opportunity for calculus formation.
-
Oral Hygiene Practices: This is undeniably the most crucial factor. Anyone who doesn’t brush and floss thoroughly and regularly is highly susceptible to calculus development.
-
Other Contributing Factors: These can include smoking, crowded teeth (which are harder to clean), and certain medications that cause dry mouth.
The Damaging Effects of Dental Calculus
Here, it’s absolutely vital that we help our patients understand that the problem extends far beyond mere aesthetics. Dental calculus, and critically, the active plaque biofilm that perpetually covers it, is the primary culprit behind:
-
Gingivitis: The initial stage, where gums become red, swollen, and bleed easily.
-
Periodontitis: If gingivitis is left untreated, the inflammation progressively extends down to the bone and ligaments surrounding the tooth.
-
Bone Loss: The bacteria and their destructive toxins relentlessly break down the bone supporting the tooth.
-
Tooth Mobility: As bone support diminishes, the tooth inevitably begins to loosen and move.
-
Tooth Loss: Ultimately, the tooth loses its entire support structure and must be extracted.
Conclusion: Calculus is No Friend
Dental calculus is not merely a cosmetic concern; it represents a serious health issue that starts small but can tragically culminate in tooth loss. Our unwavering role as dentists is to serve as the first line of defense. This means not only meticulously removing calculus but, just as importantly, educating and empowering our patients. They need to understand that diligent brushing, consistent flossing, and regular visits to the clinic are their only true weapons against this silent adversary.